扩展功能
文章信息
- 迟小惠, 冯友军, 郑焙文
- CHI Xiao-Hui, FENG You-Jun, ZHENG Bei-Wen
- 耐药菌在人-动物-环境中的传播和遗传机制
- Transmission and genetic mechanism of drug-resistant bacteria in multi-sectors
- 微生物学通报, 2019, 46(2): 311-318
- Microbiology China, 2019, 46(2): 311-318
- DOI: 10.13344/j.microbiol.china.180864
-
文章历史
- 收稿日期: 2018-11-01
- 接受日期: 2019-01-04
- 网络首发日期: 2019-01-09
2. 浙江大学医学院/动物科学学院 浙江 杭州 310058;
3. 浙江大学医学院附属第一医院 感染性疾病诊治协同创新中心 传染病诊治国家重点实验室 浙江 杭州 310003
2. School of Medicine and College of Animal Sciences, Zhejiang University, Hangzhou, Zhejiang 310058, China;
3. Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, the First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, Zhejiang 310003, China
单细胞生物(细菌和古生菌)是最早出现在地球上的生命形式,可以追溯到38亿年前。在早期阶段,细菌在极其恶劣且缺氧的环境中进化,并暴露在强烈的太阳辐射和广泛的火山活动带来的高温下。因此,细菌进化成为耐寒、适应性强的生物,从那时起,细菌便广泛存在于生态系统中[1]。自20世纪20年代末弗莱明发现青霉素以来,将抗生素应用于人类医学被公认为有史以来最伟大的医学进步[2]。然而,在抗生素问世不到80年的时间里,人类过度使用抗生素,施加的选择压力有利于耐药菌的存活,进一步加剧了耐药性的出现和扩散。2016年,《二十国集团领导人杭州峰会公报》指出:抗生素耐药性严重威胁公共健康、经济增长和全球经济稳定。二十国集团峰会将推动谨慎使用抗生素,并考虑在抗生素可负担和可获得性方面的巨大挑战及其对公共卫生的影响,采取包容的方式应对抗生素耐药性问题,以实证方法预防和减少抗生素耐药性,同时推动研发新的和现有的抗生素。这意味着抗生素耐药问题已经上升到了国际高度,成为一个等同于气候变化和恐怖主义的全球性问题。
细菌耐药可以引起患者使用抗生素后效果不明显,医治难度增加甚至病死率升高等严重后果[3]。进入21世纪以来,多种病原菌出现了耐药株(Drug-resistant strain)、多重耐药株(Multi-drug resistant strain),甚至泛耐药株(Pan-drug resistant strain),又称全耐药株,给人医和兽医临床带来巨大挑战。世界卫生组织(World Health Organization)也已把细菌耐药列为威胁人类健康的三大公共卫生问题之一,并在2011年世界卫生日呼吁全球采取行动,急需遏制细菌耐药[4]。
1 我国的细菌耐药现状 1.1 我国临床细菌耐药现状我国是抗生素的生产和使用大国,也存在抗菌药物使用不合理,抗生素可以随意购买的现象,从而导致了临床细菌耐药的严峻形势。近年来,我国的细菌耐药问题日趋严重,随着科研水平的不断提高,各种各样的耐药基因相继被检测到。根据卫生部全国细菌耐药监测网(Mohnarin)监测结果,全球普遍公认的多重耐药(Multi-drug resistant,MDR)与泛耐药(Pan-drug resistant,PDR)细菌十分普遍,耐甲氧西林金黄色葡萄球菌、产超广谱β-内酰胺酶的大肠埃希氏菌和耐碳青霉烯类肺炎克雷伯菌的患病率估计值(即每种细菌的所有临床分离株的比例)分别为44.6%、62%和10.5%。而国际医学界公认的“超级耐药菌”在我国十分普遍,对碳青霉烯类抗生素耐药的大肠埃希氏菌和肺炎克雷伯菌已经达到1.4%和6.8%,泛耐药不动杆菌在40%以上[5-6]。面对多重耐药和泛耐药菌感染的不断增加,临床在治疗细菌感染时面临用药选择余地有限,甚至无药可用的状况。当下,碳青霉烯类抗菌药物和黏菌素被认为是治疗多重耐药的革兰阴性菌株的最后一道防线,碳青霉烯类药物和黏菌素的耐药性也成为了当下研究的热点。2015年,质粒介导的黏菌素耐药菌株首次被发现[7],表明最后一道防线被突破,给人类健康带来严重威胁[8-9]。有研究表明,截至2016年底,我国携带mcr-1的大肠埃希氏菌的感染率为3.7%−32.7% (平均值为15.0%),大大高于此前报道的水平[10],如此之高的感染率无疑再次给人们敲响警钟。
1.2 我国动物源性细菌耐药现状动物病原菌是各类耐药基因的主要储库之一,并且可以通过食物链不断地传播给人类,成为一个危害公共安全的重大隐患[11]。在动物生产中,长期在动物饲料中添加低剂量的抗菌药物作为生长促进剂在许多国家包括中国都十分常见,这种做法在增加经济效益的同时也给公共安全问题带来巨大威胁,不断使用的抗菌剂促进并加剧了耐药菌的出现。目前,全球畜牧业生产快速增长,且集约化生产越来越普遍,其中抗菌药物的使用是畜牧业生产的一个重要环节,预计抗菌药的使用在未来增长的三分之二将用于动物生产[12]。在我国,一半以上的抗生素被用于动物养殖业。有研究对36种抗生素的使用量进行了调查,结果显示总使用量(92 700 t)中的84%是用于动物养殖业(猪52.2%,鸡19.6%,其他动物12.5%),而人的使用量仅占16%[13]。2015年,首次在中国动物体内分离了质粒介导的黏菌素耐药菌株。这些黏菌素耐药菌株的质粒上都携带了一个编码乙醇胺转移酶的新基因mcr-1,磷酸乙醇胺转移酶降低了黏菌素和脂多糖亲和性,从而导致细菌对黏菌素不敏感[7]。有研究收集了2015−2016年我国8个省份480个动物粪便样本,mcr-1阳性率为51%[14],而另有研究收集了2016−2017年我国18个省份600个动物粪便样本,mcr-1阳性率为76.2%[15]。由此可见,遏制细菌耐药已刻不容缓。
1.3 我国环境细菌耐药现状伴随着人类活动以及农业的发展,在物理和生物作用力之下,医疗行业和养殖业对环境产生了很大的负面影响,抗生素成为环境中检出频率最高的一类新型污染物之一,抗生素环境污染问题已成为国内外的研究热点。因多数抗生素在动物体内都不能代谢完全,大约30%−90%以原形或初级代谢产物的形式随动物粪便和尿液排出体外[16-17],因此,抗生素可随动物粪便或尿液大量释放到自然生态环境中,影响环境微生物种群的结构和活性[18-19]。除了抗生素,自然环境的改变也会导致细菌耐药性的进化[2]。自然环境为微生物提供了一个天然的耐药基因库,人类的活动、环境的改变、动物的迁徙等都可能影响细菌的进化,产生新的耐药基因[20]。近年来,在多种环境介质中均检测到了耐药基因的存在,包括土壤、水和蔬菜等[21-23]。环境中存在的携带mcr-1基因的耐药菌同样不容忽视。有研究调查了长江下游、附近污水处理厂和饮用水处理厂两种超级耐药基因mcr-1和blaNDM-1及其宿主细菌的流行和抗生素耐受性特征。研究结果表明mcr-1和blaNDM-1在污水处理厂的进水和生物单元中普遍存在。在长江中,检测到mcr-1和blaNDM-1具有比污水处理厂出水端更高的丰度和抗生素耐受性。这两种超级耐药基因被运送至饮用水处理厂进而转移到人体内,从而对公共健康构成巨大威胁[24]。
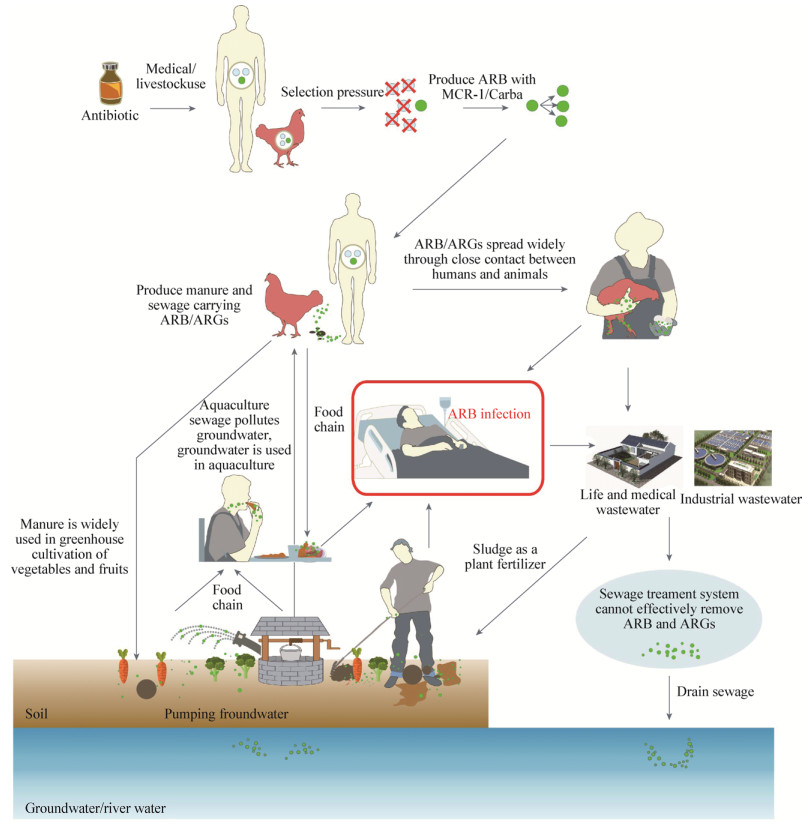
2 耐药菌在人、动物和环境中的传播和遗传机制医疗行业、动物养殖、自然环境三者在耐药菌的传播和发展中是相互影响、互相作用的有机整体(图 1)。抗生素耐药性的产生在人与动物中愈演愈烈[25-28]。动物身上的细菌对抗生素耐药会直接影响到它们的健康,食用动物可能是耐药细菌和相关耐药基因的一个聚集库[29]。而携带mcr-1的肠杆菌科细菌可以很好地适应各种宿主,并在环境、动物和人类之间传播。2015年,首次在中国动物体内分离了携带mcr-1基因的质粒介导的黏菌素耐药菌株[7, 30-32]。不仅是动物,近年来陆续从人体内分离到携带mcr-1基因的质粒介导的黏菌素耐药菌株[33-34]。同样,我们赖以生存的环境中也检测到了携带mcr-1基因的黏菌素耐药菌株。在食用家禽养殖场周围的环境中,几种不常见的肠杆菌科细菌存在mcr-1及其突变体。研究发现mcr-1位于这些细菌大小不同的质粒上,而质粒一旦进入大肠埃希氏菌宿主则可转移性增加,加速mcr-1的传播。这些环境中不常见的肠杆菌科细菌可以作为mcr-1的储存库,对人类的健康以及畜牧业都带来巨大的风险[35]。我们对山东农村地区的人群-环境-动物流行病调查发现,在山东农村的井水中也存在携带mcr-1基因的质粒介导的大肠埃希氏菌菌株。而且,在同一地区的井水中还发现了携带blaKPC-2的解尿氨酸拉乌尔菌[36]。不仅如此,我们还观察了来自农田土壤的53株(22.6%)产ESBL的肠杆菌科细菌,发现来自牲畜密集区的6株mcr-1阳性大肠埃希氏菌菌株[37]。在我国的农村地区,地下水和河水是人和家畜的灌溉用水和饮用水的主要来源。地下水和河水又容易受到人为活动的影响,会增加耐抗生素细菌从环境传播到人类和动物的风险。而且,在中国动物养殖区,由于缺少畜禽粪便的处理设施,导致直接排放到土壤环境,同时耐药菌也跟随畜禽粪便一同进入土壤,从而污染地下水。因此,在中国目前的养殖模式下,对畜禽废弃物的不恰当处置会导致周边环境介质中出现携带mcr-1基因的质粒介导的黏菌素耐药菌株。此外,我们研究发现,从井水中分离的携带mcr-1和blaCTX-M基因的两株大肠埃希氏菌属于ST10,ST10复合体是中国东南部人粪便中发现的最常见的大肠埃希氏菌序列型[38]。ST10也是人群、动物及环境等各介质中的肠杆菌科细菌的主要序列型别[39-40],且该型别与人类和动物感染密切有关,从而间接证明了人体内的耐药菌可污染环境,而水体则是耐药菌储存及传播过程中的重要环境介质。具有黏菌素抗性的菌株在人群中的流行率也不容小觑,我们多次从病人体内分离到同时携带黏菌素抗性基因mcr-1以及碳青霉烯酶抗性基因blaNDM[41-42]的耐药菌。2016年我们从一名急性肝损伤的病人体内分离出来同时携带mcr-1以及blaNDM-5的大肠埃希氏菌,且MLST分型为ST206[41]。最近从杭州市环境水样中分离出了产MCR-1的大肠埃希氏菌ST206菌株[43]。由此可见,环境与临床菌株联系紧密,临床使用黏菌素对环境等的影响仍然需要密切的关注。
|
| 图 1 耐药菌/耐药基因在人-动物-环境中的传播 Figure 1 Dissemination of drug-resistant bacteria/drug resistance genes in human-animal-environment 注:ARB:耐药菌;ARGs:耐药基因. Note: ARB: Antibiotic resistant bacteria; ARGs: Antibiotic resistance genes. |
|
|
近年来,mcr-2、mcr-3、mcr-4、mcr-5以及mcr-7等mcr-1的多种突变体也相继被发现[30-31, 44-51]。mcr-2与mcr-1一样,可通过磷酸乙醇胺转移酶催化磷酸乙醇胺添加到脂质A4位上的磷酸基团导致黏菌素耐药[45, 48]。随着mcr-1不断被检出,人们发现多个可移动元件包括质粒、转座子、插入序列都与mcr-1的转移有着密切的联系[52-53]。至今发现的可携带mcr-1的质粒类型主要包括IncI2、IncX4、IncHI2等,IncX3-IncX4和IncI2-IncFIB等杂合质粒也参与其中[50, 54-55],甚至在染色体上携带的mcr-1也有诸多报道[56]。此外,携带mcr-1的质粒非常稳定,即使没有黏菌素的选择性压力,也会稳定存在并广泛传播。以IncX4质粒为主线,系统分析mcr-1的基因环境,发现mcr-1的转座与ISApl1密切相关[57]。此外,IncX4与IncI2型质粒为人群中携带mcr-1的主要型别质粒[14],且有研究证实这两种型别的质粒可在人体肠道内稳定遗传并表达,对控制mcr-1的传播有巨大影响[58]。而且,我们在单一分离株中检测到同时出现两个独特的携带mcr-1的质粒IncI2和IncX4,这可能加速了环境选择压力下mcr-1的传播[54]。IncF和IncN型质粒也有在人体的检出报道[59],因此,所有携带mcr-1的质粒类型都需要得到重视。通过对GenBank中携带mcr-1的序列进行分析,研究者发现转座子Tn6330在mcr-1的传播过程中发挥重要作用[60]。
3 细菌耐药的防控策略 3.1 发动多学科联动应对细菌耐药问题耐药基因可以在人、动物和环境中循环传播,增加了人类摄入耐药基因的风险[61],这种风险既是医学问题,也是生态学问题[62-63]。耐药基因可能通过食物链或者致病菌传递给人体,其潜在的威胁已经引起了社会各界的广泛重视和关注。面对这类问题,传统单一化的卫生工作系统已很难有效地解决这类挑战,急需多学科、多领域的合作来共同应对和解决目前公共卫生方面存在的问题。这就要求我们必须从人类、动物和环境因素的综合角度出发,以创新的方式思考健康问题。“大健康”策略致力于结合医学、兽医学和环境科学,以改善人和动物生存、生活质量为理念呼吁人类卫生保健的提供者、公共卫生专业人员和兽医之间加强交流与合作,从而更好地解决此类新发问题[64]。
3.2 充分发挥政府的引导和监管功能政府部门应加强宣传与教育,监控抗生素使用和耐药产生情况,鼓励和投入更多专项经费资助科学家研究耐药菌的产生、传播和进化机制[65]。建立有效的兽医耐药性监测网络是获得耐药性基础数据的前提,也是耐药性风险评估以及防控的科学依据。同时网络的交流平台还可传播耐药性理论、检测标准和技术服务,并融入到养殖业控制体系[66]。同时,政府管理部门需要站在全球的高度认识细菌耐药,制定相关管理法规,实施耐药控制计划,控制耐药不仅仅只停留在口号,需要实际可行的计划,多部门联动,在管理方式方法等方面达成一致,才能真正有效地遏制细菌耐药[4]。二十国集团峰会后,我国14个部门联合印发了《遏制细菌耐药国家行动计划》,旨在从国家层面实施综合治理策略和措施,对抗菌药物的研发、生产、流通、应用、环境保护等各个环节加强监管,加强宣传教育和国际交流合作,应对细菌耐药带来的风险和挑战[32, 67]。
3.3 建立控制细菌耐药的技术支撑体系及时掌握细菌耐药流行情况以及相关信息,对合理使用抗菌药物和遏制细菌耐药具有十分重要的价值。细菌耐药监测需要成为立体化网络,包括各个层面和各个地区的耐药信息采集。目前急需建立不同层次不同领域共同的监测体系,各领域所获得的信息互相配合,各自发挥不同作用,共同应对细菌耐药。与此同时,还应重视与细菌耐药监测相匹配的抗菌药物生产、流通、应用监测体系,对掌握药品消费状况、合理应用现状等具有重要意义[4]。
3.4 加强科普知识宣传,提高民众对抗菌药物合理使用与细菌耐药的认识广泛宣传抗菌药物合理使用的知识,提高社会公众和医务人员对细菌耐药危机的认识。牢固树立抗菌药物合理使用观念,减少不必要的药物使用,让全社会都来关心、支持和参与抗菌药物的合理使用。切实维护患者用药权益,保障医疗质量和医疗安全,合理、规范使用抗菌药物。
| [1] |
Dodd MS, Papineau D, Grenne T, et al. Evidence for early life in Earth's oldest hydrothermal vent precipitates[J]. Nature, 2017, 543(7643): 60-64. DOI:10.1038/nature21377 |
| [2] |
Wang YN, Hu YF, Zhu BL, et al. Antibiotic resistome in farm animals and their related environments: a review[J]. Chinese Journal of Biotechnology, 2018, 34(8): 1226-1233. (in Chinese) 王亚楠, 胡永飞, 朱宝利, 等. 养殖动物及其相关环境耐药组的研究进展[J]. 生物工程学报, 2018, 34(8): 1226-1233. |
| [3] |
Zhu YG, Johnson TA, Su JQ, et al. Diverse and abundant antibiotic resistance genes in Chinese swine farms[J]. Proceedings of the National Academy of Sciences of the United States of America, 2013, 110(9): 3435-3440. DOI:10.1073/pnas.1222743110 |
| [4] |
Xiao YH. Bacterial resistance: challenge and strategies[J]. China Licensed Pharmacist, 2011, 8(6): 3-8. (in Chinese) 肖永红. 细菌耐药:挑战与对策[J]. 中国执业药师, 2011, 8(6): 3-8. DOI:10.3969/j.issn.1672-5433.2011.06.001 |
| [5] |
Viau R, Frank KM, Jacobs MR, et al. Intestinal carriage of carbapenemase-producing organisms: current status of surveillance methods[J]. Clinical Microbiology Reviews, 2016, 29(1): 1-27. DOI:10.1128/CMR.00108-14 |
| [6] |
Committee of Experts on Rational Drug Use, National Health and Family Planning Commission of the P. R. China, China Antimicrobial Resistance Surveillance System. China antimicrobial resistance surveillance system report 2015[J]. China Licensed Pharmacist, 2016, 13(3): 3-8. (in Chinese) 国家卫生计生委合理用药专家委员会, 全国细菌耐药监测网. 2015年全国细菌耐药监测报告[J]. 中国执业药师, 2016, 13(3): 3-8. DOI:10.3969/j.issn.1672-5433.2016.03.001 |
| [7] |
Liu YY, Wang Y, Walsh TR, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study[J]. The Lancet Infectious Diseases, 2016, 16(2): 161-168. DOI:10.1016/S1473-3099(15)00424-7 |
| [8] |
Caselli E, D'Accolti M, Soffritti I, et al. Spread of mcr-1-driven colistin resistance on hospital surfaces, Italy[J]. Emerging Infectious Diseases, 2018, 24(9): 1752-1753. DOI:10.3201/eid2409.171386 |
| [9] |
Kurekci C, Aydin M, Nalbantoglu OU, et al. The first report of mobile colistin resistance gene (mcr-1) carrying Escherichia coli in Turkey[J]. Journal of Global Antimicrobial Resistance, 2018, 15: 169-170. DOI:10.1016/j.jgar.2018.09.013 |
| [10] |
Shen YB, Zhou HW, Xu J, et al. Anthropogenic and environmental factors associated with high incidence of mcr-1 carriage in humans across China[J]. Nature Microbiology, 2018, 3(9): 1054-1062. DOI:10.1038/s41564-018-0205-8 |
| [11] |
Carattoli A. Animal reservoirs for extended spectrum β-lactamase producers[J]. Clinical Microbiology and Infection, 2008, 14(S1): 117-123. |
| [12] |
van Boeckel TP, Brower C, Gilbert M, et al. Global trends in antimicrobial use in food animals[J]. Proceedings of the National Academy of Sciences of the United States of America, 2015, 112(18): 5649-5654. DOI:10.1073/pnas.1503141112 |
| [13] |
Zhang QQ, Ying GG, Pan CG, et al. Comprehensive evaluation of antibiotics emission and fate in the river basins of China: source analysis, multimedia modeling, and linkage to bacterial resistance[J]. Environmental Science & Technology, 2015, 49(11): 6772-6782. |
| [14] |
Chen KC, Chan EWC, Xie MM, et al. Widespread distribution of mcr-1-bearing bacteria in the ecosystem, 2015 to 2016[J]. Eurosurveillance, 2017, 22(39): 17-00206. |
| [15] |
Tong HX, Liu JX, Yao XH, et al. High carriage rate of mcr-1 and antimicrobial resistance profiles of mcr-1-positive Escherichia coli isolates in swine faecal samples collected from eighteen provinces in China[J]. Veterinary Microbiology, 2018, 225: 53-57. DOI:10.1016/j.vetmic.2018.09.018 |
| [16] |
Aust MO, Godlinski F, Travis GR, et al. Distribution of sulfamethazine, chlortetracycline and tylosin in manure and soil of Canadian feedlots after subtherapeutic use in cattle[J]. Environmental Pollution, 2008, 156(3): 1243-1251. DOI:10.1016/j.envpol.2008.03.011 |
| [17] |
Sarmah AK, Meyer MT, Boxall ABA. A global perspective on the use, sales, exposure pathways, occurrence, fate and effects of veterinary antibiotics (VAs) in the environment[J]. Chemosphere, 2006, 65(5): 725-759. DOI:10.1016/j.chemosphere.2006.03.026 |
| [18] |
Martinez JL. Environmental pollution by antibiotics and by antibiotic resistance determinants[J]. Environmental Pollution, 2009, 157(11): 2893-2902. DOI:10.1016/j.envpol.2009.05.051 |
| [19] |
Martinez JL. The role of natural environments in the evolution of resistance traits in pathogenic bacteria[J]. Proceedings of the Royal Society B: Biological Sciences, 2009, 276(1667): 2521-2530. DOI:10.1098/rspb.2009.0320 |
| [20] |
Cheng DM, Feng Y, Liu YW, et al. Dynamics of oxytetracycline, sulfamerazine, and ciprofloxacin and related antibiotic resistance genes during swine manure composting[J]. Journal of Environmental Management, 2019, 230: 102-109. |
| [21] |
Ben Said L, Jouini A, Klibi N, et al. Detection of extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae in vegetables, soil and water of the farm environment in Tunisia[J]. International Journal of Food Microbiology, 2015, 203: 86-92. DOI:10.1016/j.ijfoodmicro.2015.02.023 |
| [22] |
Yang FX, Zhang KQ, Zhi SL, et al. High prevalence and dissemination of β-lactamase genes in swine farms in northern China[J]. Science of the Total Environment, 2019, 651: 2507-2513. DOI:10.1016/j.scitotenv.2018.10.144 |
| [23] |
Abera B, Kibret M, Mulu W. Extended-spectrum beta (β)-lactamases and antibiogram in enterobacteriaceae from clinical and drinking water sources from Bahir Dar City, Ethiopia[J]. PLoS One, 2016, 11(11): e0166519. DOI:10.1371/journal.pone.0166519 |
| [24] |
Wang RN, Zhang Y, Cao ZH, et al. Occurrence of super antibiotic resistance genes in the downstream of the Yangtze River in China: Prevalence and antibiotic resistance profiles[J]. Science of the Total Environment, 2019, 651: 1946-1957. DOI:10.1016/j.scitotenv.2018.10.111 |
| [25] |
van den Bergh B, Michiels JE, Wenseleers T, et al. Frequency of antibiotic application drives rapid evolutionary adaptation of Escherichia coli persistence[J]. Nature Microbiology, 2016, 1: 16020. DOI:10.1038/nmicrobiol.2016.20 |
| [26] |
Reding-Roman C, Hewlett M, Duxbury S, et al. The unconstrained evolution of fast and efficient antibiotic-resistant bacterial genomes[J]. Nature Ecology & Evolution, 2017, 1(3): 0050. |
| [27] |
Ding SJ, Han XH, Li J, et al. Discovery of multi-drug resistant, MCR-1 and ESBL-coproducing ST117Escherichia coli from diseased chickens in Northeast China[J]. Science Bulletin, 2018, 63(16): 1059-1066. DOI:10.1016/j.scib.2018.07.017 |
| [28] |
Zhang HM, Seward CH, Wu ZW, et al. Genomic insights into the ESBL and MCR-1-producing ST648Escherichia coli with multi-drug resistance[J]. Science Bulletin, 2016, 61(11): 875-878. DOI:10.1007/s11434-016-1086-y |
| [29] |
Pruden A, Pei RT, Storteboom H, et al. Antibiotic resistance genes as emerging contaminants: studies in northern Colorado[J]. Environmental Science & Technology, 2006, 40(23): 7445-7450. |
| [30] |
Gao RS, Hu YF, Li ZC, et al. Dissemination and mechanism for the MCR-1 colistin resistance[J]. PLoS Pathogens, 2016, 12(11): e1005957. DOI:10.1371/journal.ppat.1005957 |
| [31] |
Wei WH, Srinivas S, Lin JX, et al. Defining ICR-Mo, an intrinsic colistin resistance determinant from Moraxella osloensis[J]. PLoS Genetics, 2018, 14(5): e1007389. DOI:10.1371/journal.pgen.1007389 |
| [32] |
Wang XN, Zhang HM, Sun J, et al. The MCR-1 colistin resistance: a new challenge to global public health[J]. Chinese Science Bulletin, 2017, 62(10): 1018-1029. DOI:10.1360/N972016-01084 |
| [33] |
Cao L, Li XM, Xu Y, et al. Prevalence and molecular characteristics of mcr-1 colistin resistance in Escherichia coli: isolates of clinical infection from a Chinese University Hospital[J]. Infection and Drug Resistance, 2018, 11: 1597-1603. DOI:10.2147/IDR |
| [34] |
Pillonetto M, Mazzetti A, Becker GN, et al. Low level of polymyxin resistance among nonclonal mcr-1-positive Escherichia coli from human sources in Brazil[J]. Diagnostic Microbiology and Infectious Disease, 2019, 93(2): 140-142. DOI:10.1016/j.diagmicrobio.2018.08.009 |
| [35] |
Wang XM, Wang Y, Wang Y, et al. Emergence of the colistin resistance gene mcr-1 and its variant in several uncommon species of Enterobacteriaceae from commercial poultry farm surrounding environments[J]. Veterinary Microbiology, 2018, 219: 161-164. DOI:10.1016/j.vetmic.2018.04.002 |
| [36] |
Sun P, Bi ZW, Nilsson M, et al. Occurrence of blaKPC-2, blaCTX-M, and mcr-1 in Enterobacteriaceae from well water in rural China[J]. Antimicrobial Agents and Chemotherapy, 2017, 61(4): e02569-16. |
| [37] |
Zheng BW, Huang C, Xu H, et al. Occurrence and genomic characterization of ESBL-producing, MCR-1-harboring Escherichia coli in farming soil[J]. Frontiers in Microbiology, 2017, 8: 2510. DOI:10.3389/fmicb.2017.02510 |
| [38] |
Chen Y, Chen X, Zheng S, et al. Serotypes, genotypes and antimicrobial resistance patterns of human diarrhoeagenic Escherichia coli isolates circulating in southeastern China[J]. Clinical Microbiology and Infection, 2014, 20(1): 52-58. DOI:10.1111/1469-0691.12188 |
| [39] |
Zhang YW, Liao K, Gao H, et al. Wang, H. Wang. Decreased fitness and virulence in ST10Escherichia coli harboring blaNDM-5 and mcr-1 against a ST4981 strain with blaNDM-5[J]. Frontiers in Cellular and Infection Microbiology, 2017, 7: 242. DOI:10.3389/fcimb.2017.00242 |
| [40] |
Fernandes MR, Sellera FP, Esposito F, et al. Colistin-resistant mcr-1-positive Escherichia coli on public beaches, an infectious threat emerging in recreational waters[J]. Antimicrobial Agents and Chemotherapy, 2017, 61(7): e00234-17. |
| [41] |
Zheng BW, Lv T, Xu H, et al. Discovery and characterisation of an Escherichia coli ST206 strain producing NDM-5 and MCR-1 from a patient with acute diarrhoea in China[J]. International Journal of Antimicrobia Agents, 2018, 51(2): 273-275. DOI:10.1016/j.ijantimicag.2017.09.005 |
| [42] |
Zheng BW, Yu X, Xu H, et al. Complete genome sequencing and genomic characterization of two Escherichia coli strains co-producing MCR-1 and NDM-1 from bloodstream infection[J]. Scientific Reports, 2017, 7(1): 17885. DOI:10.1038/s41598-017-18273-2 |
| [43] |
Zhou HW, Zhang T, Ma JH, et al. Occurrence of plasmid- and chromosome-carried mcr-1 in waterborne Enterobacteriaceae in China[J]. Antimicrobial Agents and Chemotherapy, 2017, 61(8): e0001-17. |
| [44] |
Xavier BB, Lammens C, Ruhal R, et al. Identification of a novel plasmid-mediated colistin-resistance gene, mcr-2, in Escherichia coli, Belgium, June 2016[J]. Eurosurveillance, 2016, 21(27): 30280. DOI:10.2807/1560-7917.ES.2016.21.27.30280 |
| [45] |
Xu YC, Lin JX, Cui T, et al. Mechanistic insights into transferable polymyxin resistance among gut bacteria[J]. The Journal of Biological Chemistry, 2018, 293(12): 4350-4365. DOI:10.1074/jbc.RA117.000924 |
| [46] |
Teo JWP, Kalisvar M, Venkatachalam I, et al. mcr-3 and mcr-4 variants in carbapenemase-producing clinical Enterobacteriaceae do not confer phenotypic polymyxin resistance[J]. Journal of Clinical Microbiology, 2018, 56(3): e01562-17. |
| [47] |
Sun J, Xu YC, Gao RS, et al. Deciphering MCR-2 colistin resistance[J]. mBio, 2017, 8(3): e00625-17. |
| [48] |
Xu YC, Wei WH, Lei S, et al. An evolutionarily conserved mechanism for intrinsic and transferable polymyxin resistance[J]. mBio, 2018, 9(2): e02317--17. |
| [49] |
Ye HY, Li YH, Li ZC, et al. Diversified mcr-1-harbouring plasmid reservoirs confer resistance to colistin in human gut microbiota[J]. mBio, 2016, 7(2): e00177-16. |
| [50] |
Sun J, Zhang HM, Liu YH, et al. Towards understanding MCR-like colistin resistance[J]. Trends in Microbiology, 2018, 26(9): 794-808. DOI:10.1016/j.tim.2018.02.006 |
| [51] |
Xu YC, Zhong LL, Srinivas S, et al. Spread of MCR-3 colistin resistance in China: An epidemiological, genomic and mechanistic study[J]. EBioMedicine, 2018, 34: 139-157. DOI:10.1016/j.ebiom.2018.07.027 |
| [52] |
Wang RB, van Dorp L, Shaw V, et al. The global distribution and spread of the mobilized colistin resistance gene mcr-1[J]. Nature Communications, 2018, 9(1): 1179. |
| [53] |
Wang QJ, Li ZC, Lin JX, et al. Complex dissemination of the diversified mcr-1-harbouring plasmids in Escherichia coli of different sequence types[J]. Oncotarget, 2016, 7(50): 82112-82122. |
| [54] |
Wang QJ, Sun J, Li J, et al. Expanding landscapes of the diversified mcr-1-bearing plasmid reservoirs[J]. Microbiome, 2017, 5(1): 70. DOI:10.1186/s40168-017-0288-0 |
| [55] |
Feng YJ. Transferability of MCR-1/2 polymyxin resistance: complex dissemination and genetic mechanism[J]. ACS Infectious Diseases, 2018, 4(3): 291-300. DOI:10.1021/acsinfecdis.7b00201 |
| [56] |
Sun J, Li XP, Fang V, et al. Co-occurrence of mcr-1 in the chromosome and on an IncHI2 plasmid: persistence of colistin resistance in Escherichia coli[J]. International Journal of Antimicrobial Agents, 2018, 51(6): 842-847. DOI:10.1016/j.ijantimicag.2018.01.007 |
| [57] |
Sun J, Fang LX, Wu ZW, et al. Genetic analysis of the IncX4 plasmids: implications for a unique pattern in the mcr-1 acquisition[J]. Scientific Reports, 2017, 7: 424. DOI:10.1038/s41598-017-00095-x |
| [58] |
Matamoros S, van Hattem JM, Arcilla MS, et al. Global phylogenetic analysis of Escherichia coli and plasmids carrying the mcr-1 gene indicates bacterial diversity but plasmid restriction[J]. Scientific Reports, 2017, 7(1): 15364. DOI:10.1038/s41598-017-15539-7 |
| [59] |
Wang J, Yuan M, Chen H, et al. First report of Klebsiella oxytoca strain simultaneously producing NDM-1, IMP-4, and KPC-2 carbapenemases[J]. Antimicrobial Agents and Chemotherapy, 2017, 61(9): e00877-17. |
| [60] |
Snesrud E, McGann P, Chandler M. The birth and demise of the ISApl1-mcr-1-ISApl1 composite transposon: the vehicle for transferable colistin resistance[J]. mBio, 2018, 9(1): e0238-17. |
| [61] |
Hu YF, Yang X, Li J, et al. The bacterial mobile resistome transfer network connecting the animal and human microbiomes[J]. Applied and Environmental Microbiology, 2016, 82(22): 6672-6681. DOI:10.1128/AEM.01802-16 |
| [62] |
Hu YF, Gao GF, Zhu BL. The antibiotic resistome: gene flow in environments, animals and human beings[J]. Frontiers of Medicine, 2017, 11(2): 161-168. DOI:10.1007/s11684-017-0531-x |
| [63] |
Woolhouse M, Ward M, van Bunnik B, et al. Antimicrobial resistance in humans, livestock and the wider environment[J]. Philosophical Transactions of the Royal Society B: Biological Sciences, 2015, 370(1670): 20140083. DOI:10.1098/rstb.2014.0083 |
| [64] |
Mwangi W, de Figueiredo P, Criscitiello MF. One health: addressing global challenges at the nexus of human, animal, and environmental health[J]. PLoS Pathogens, 2016, 12(9): e1005731. DOI:10.1371/journal.ppat.1005731 |
| [65] |
Yin YS, Chen HH, Cao LY, et al. Progress in strategies to combat antimicrobial resistance[J]. Chinese Journal of Biotechnology, 2018, 34(8): 1346-1360. (in Chinese) 尹业师, 陈华海, 曹林艳, 等. 细菌耐药性应对策略研究进展[J]. 生物工程学报, 2018, 34(8): 1346-1360. |
| [66] |
Sun J, Liu YH, Feng YJ. Towards understanding antibiotic resistance in animals-borne bacterial pathogens[J]. Chinese Journal of Biotechnology, 2018, 34(8): 1246-1258. (in Chinese) 孙坚, 刘雅红, 冯友军. 动物源细菌耐药性研究现状与对策[J]. 生物工程学报, 2018, 34(8): 1246-1258. |
| [67] |
Xiao YH, Li LJ. China's national plan to combat antimicrobial resistance[J]. The Lancet Infectious Diseases, 2016, 16(11): 1216-1218. DOI:10.1016/S1473-3099(16)30388-7 |
 2019, Vol. 46
2019, Vol. 46




